How Nervous, Endocrine, and Immune Systems Orchestrate the Response to Injury
Imagine a world where a simple paper cut could lead to life-threatening consequences. Fortunately, our bodies have evolved intricate systems that work in harmony to protect us from such scenarios. When injury occurs, our nervous, endocrine, and immune systems spring into action, engaging in a complex dance to defend and heal our bodies. This intricate response involves a myriad of chemical messengers, feedback loops, and cross-system communication. The coordinated action of these systems not only addresses the immediate threat but also sets the stage for long-term recovery and adaptation.
Fine Tuned Systems
Understanding the interplay between these systems is crucial for developing effective strategies to manage pain, promote healing, and prevent chronic conditions. This knowledge can help us unravel the mysteries of chronic pain and other conditions that arise from dysregulation of these systems. By appreciating the complex interactions at play, we can develop more targeted and holistic approaches to patient care. This blog post explores the research article, Pain and Stress in a Systems Perspective: Reciprocal Neural, Endocrine, and Immune Interactions, and entertains the fascinating question: How do the nervous, endocrine, and immune systems work together to respond to injury and what are the implications for understanding chronic pain?
The researchers conducted an extensive literature review, synthesizing findings from various studies to create a comprehensive framework of the body's response to injury. This review encompassed research from diverse fields, including neuroscience, endocrinology, immunology, and pain medicine. The authors employed a systems-based approach to integrate findings and identify overarching principles of cross-system communication and regulation. The review encompassed a wide range of research, including studies on specific mechanisms, pathways, and interactions between the nervous, endocrine, and immune systems. Studies ranged from molecular-level investigations to clinical observations and patient-reported outcomes. The authors carefully evaluated the quality and reliability of each study before incorporating its findings into the framework.
Chronic Pain Conundrum
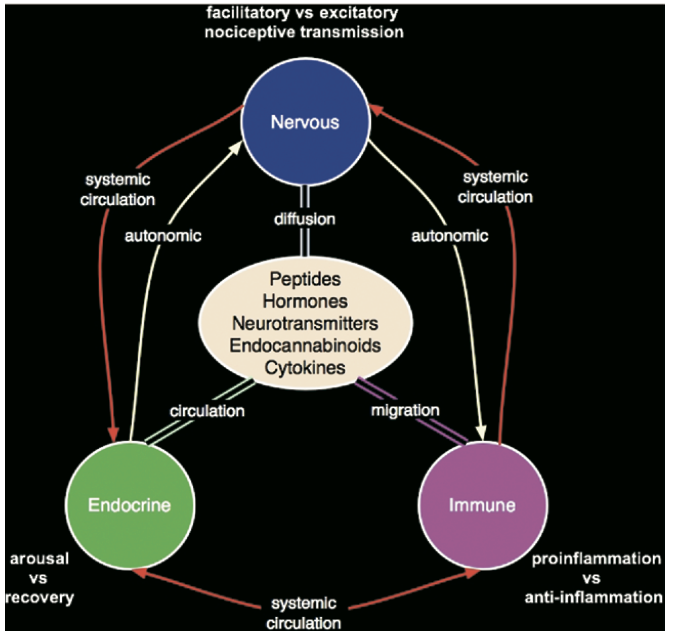
The main results of the research reveal that the nervous, endocrine, and immune systems communicate using a shared chemical language of neurotransmitters, peptides, endocannabinoids, cytokines, and hormones. This common language allows for seamless integration of signals and responses across systems. Disruptions in this chemical communication can lead to imbalances and dysregulation. These systems engage in constant feedback loops, allowing for dynamic regulation and adaptation to stressors like injury. Positive feedback loops amplify responses and enable rapid mobilization of resources to address threats, while negative feedback loops help maintain homeostasis and prevent overshooting or prolonged activation of defense mechanisms. Dysregulation of this complex interplay can contribute to the development of chronic pain conditions. Persistent inflammation, altered pain processing, and maladaptive stress responses can perpetuate pain long after the initial injury has healed. Individual differences in genetics, epigenetics, and life experiences can influence the resilience or vulnerability of these regulatory systems.
The findings suggest that chronic pain may result from a dysregulation of the nervous-endocrine-immune supersystem, rather than a localized issue. This understanding shifts the focus from treating chronic pain as a purely neurological or musculoskeletal problem to addressing systemic imbalances. The supersystem perspective opens up new avenues for research and treatment, emphasizing the need for multidisciplinary approaches. This research provides a framework for understanding the complex, multisystem nature of the body's response to injury and pain. The supersystem model integrates previously separate findings and highlights the importance of cross-system communication in health and disease. This framework can guide future research efforts, encouraging investigations that bridge traditional disciplinary boundaries.
Addressing Chronic Pain at Optimize Chiropractic
Chronic pain is complicated and continuous research that sets out to discover the complex interplay of different systems and why some individuals recover while others don’t is a key aspect of helping more people find solutions. As mentioned above altered pain processing, and maladaptive stress responses can perpetuate pain long after the initial injury. In the past we’ve discussed central sensitization which is where the nervous system becomes extra sensitive to normal movement and bodily functions this then results in pain in the absence of actual tissue damage. Central Sensitization is the altered pain processing aspect of chronic pain.
When in comes to finding a solution and improving chronic pain its key to explore the different systems that are interacting with each other in order to fully understand the dysfunction that is occurring.
For instance the majority of individuals who suffer from a whiplash injury heal and recover with no residual effects. Others have structural damage such as muscles strains or even ligament damage while others have ever deeper effects negatively affecting how the neurology of the neck works with the eyes and the inner ear. (Our eyes, our inner ear, and the sensors in our upper neck help us maintain our balance.)
Due to this fact many individuals who suffer from a whiplash injury and experience dizziness or headaches, common symptoms following a whiplash injury, will see a physical therapist, chiropractor, or other health provider and get some relief but not find long term resolution. This is why it is key to examine the systems that control balance and determine if the injury is more than just muscular and to fully understand the extent of the injury and if altered sensory processing is occurring. That’s what we do at Optimize Chiropractic by utilizing the Modified Clinical Test of Sensory Integration and Balance, by examining range of motion, and the ability to control movement with the joint position error test we are more fully able to understand the cause of the symptoms as well as create a plan of action that specifically addresses the multiple layers of dysfunction.
Chronic pain sucks and finding ways to improve it and alter it in order to live a more pain free is possible. It takes work though, both by the provider you’re working with and as the individual suffering as well, but improvement can be found.
If you’re someone who lives with chronic pain and is looking to find a solution reach out to us at 614-769-7831 to schedule your complimentary consultation or click below to find out if we can help you.
We also have many more resources available on our Youtube Page and multiple blogs on how you can play an active role in reducing your pain. Unlocking the Power of Slow Deep Breathing: A Study on Pain Reduction , Balance & Fibromyalgia, Retraining the Brain: Mindfulness, Every Little Bit Helps, Mindfulness & Chronic Pain.