The Similar Outcomes Paradox
Why Everything — and Nothing — Works for Pain
"My PT says I need to strengthen my core. My chiropractor says my spine is misaligned. My doctor wants me to try counseling. They all sound confident — but I’m more confused than ever."
If that sounds familiar, you’re not alone. I hear versions of this every week.
The reason for this is because each provider sees your pain through their own lens, offers their own solution, and leaves you stuck trying to decide who’s “right.”
But here’s what often not talked about, when scientists put these treatments to the test, they often find that multiple methods can lead to similar outcomes.
This is what I like to call the similar outcomes paradox — and it doesn’t mean everything works equally well. It means something deeper is going on. Something that can actually help you make better decisions about your recovery.
The Research You Haven’t Heard Of
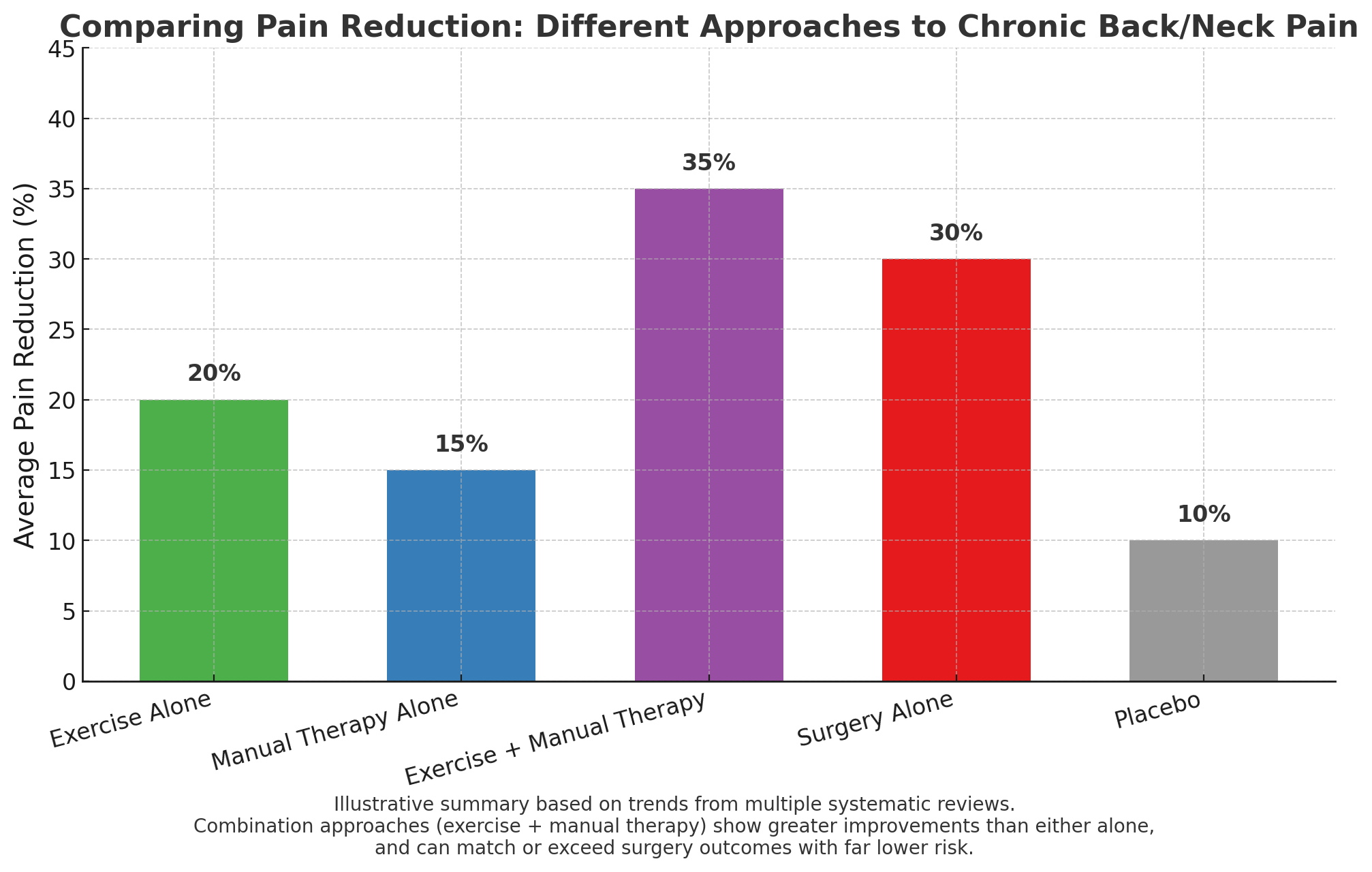
When researchers conduct high-quality studies on chronic low back pain, they often compare very different treatments — strength training, spinal manipulation, cognitive behavioral therapy, and surgery.
Here’s what they consistently find:
Exercise therapy typically improves pain by 6–8 points on a 100-point scale — a small but meaningful benefit for many people.
Manual therapy shows similar effects.
Manual therapy and Exercise combined produces even better results
Pain education and cognitive approaches also create modest improvements.
And in major trials comparing spinal fusion surgery to therapy programs that include movement and education, the long-term outcomes were the same — but surgery came with far more risk.
In other words, you can have a completely different route and end up in a similar place.
But that doesn’t mean all care is created equal. It means one specific approach isn’t what drives the majority of the benefit.
Why Would Such Different Treatments Work Equally Well?
It’s not because they’re all “just placebo.”
Each has real, measurable biological effects:
Strength training and movement retrain your nervous system, strengthen tissue tolerance and rebuild resilience.
Manual therapy stimulates your brain’s natural pain modulation systems.
Pain education changes the way your brain interprets danger and threat.
But the data suggests those effects only go so far unless they’re delivered in the right context.
The most powerful ingredients for recovery — the ones that consistently predict better outcomes across dozens of trials — aren’t tied to one specific treatment. They’re tied to how care is delivered.
What are those ingredients?
You feel heard and understood.
Your relationship with your provider isn't a side detail — it’s a core part of your recovery. Research shows it can influence outcomes as much as the treatment itself. When you feel safe, your nervous system shifts from threat mode to healing mode.You believe you can improve.
This isn’t wishful thinking. When you expect recovery, your brain releases its own version of painkillers. Your immune system changes. Your body starts moving toward safety.You’re given a clear, empowering explanation.
Effective care reframes pain from “something is broken” to “your system is sensitive, but it can change.” That shift alone reduces fear, builds confidence, and changes how your brain processes pain.
Why This Doesn’t Mean “All Treatments Are Equal”
This paradox isn’t a reason to throw your hands up and say “Nothing works.”
It’s a reason to stop chasing one specific approach — and start seeking care that understands how healing actually works.
Yes, you need methods that restore motion, improve load tolerance, and rebuild strength. But you also need someone who can deliver those tools in a way that activates the nervous system’s ability to adapt and change.
What That Looks Like in Our Clinic
This is exactly how we approach care.
Yes — I’m a chiropractor. I practice a specific hands-on technique that restores movement and reduces restriction, but we don’t stop there. Your pain isn’t one-dimensional — and your care shouldn’t be either.
Our approach includes:
Manual therapy to improve motion and decrease pain — especially early on
Pain neuroscience education integrated throughout so you understand your body, not fear it
Rehabilitation during injury — real strength training tailored to your current capacity, not just “exercises”
Balance and movement retraining to rebuild coordination and long-term control
Clinical technology to track your progress and personalize your plan
Each tool plays a role. But the power comes from how they’re combined — and from the environment we build together: one of safety, partnership, and forward movement.
Why This Matters for You
You don’t need to search endlessly for the one technique that finally fixes you.
You don’t need to bounce between specialists, hoping someone has the missing piece.
And you definitely don’t need to believe that if the first thing you tried didn’t work, it must mean you’re broken.
What you need is care that’s evidence-informed and person-centered. Care that combines what we know works biologically with what we know works neurologically and emotionally.
That’s what we do.
And it’s why we see people get better — even when they’ve tried “everything” before.
You Don’t Have Just One Option
If you’ve been told your only option is surgery…
If you’ve tried three different treatments and none of them “stuck”…
If you’re starting to wonder if maybe you just have to live with this…
You are not broken.
Your system is adaptable it just needs the right approach for you..
And your recovery is possible.
It doesn’t hinge on finding one magic fix. It hinges on receiving care that treats you like a whole person — not just a spine, a joint, or a diagnosis.
If you’re ready for care that combines proven methods with the deeper science of how healing really happens, we’re ready to help.
References
Brox JI, Sørensen R, Friis A, et al. Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine (Phila Pa 1976). 2003;28(17):1913-1921. doi:10.1097/01.BRS.0000083234.62751.7A
Coulter ID, Crawford C, Hurwitz EL, et al. Manipulation and mobilization for treating chronic low back pain: a systematic review and meta-analysis. Spine J. 2018;18(5):866-879. doi:10.1016/j.spinee.2018.01.013
Gevers-Montoro C, Romero-Santiago B, Medina-García I, et al. Reduction of Chronic Primary Low Back Pain by Spinal Manipulative Therapy is Accompanied by Decreases in Segmental Mechanical Hyperalgesia and Pain Catastrophizing: A Randomized Placebo-controlled Dual-blind Mixed Experimental Trial. J Pain. 2024;25(8):104500. doi:10.1016/j.jpain.2024.02.014
Hayden JA, Ellis J, Ogilvie R, et al. Some types of exercise are more effective than others in people with chronic low back pain: a network meta-analysis. J Physiother. 2021;67(4):252-262. doi:10.1016/j.jphys.2021.09.004
Hróbjartsson A, Gøtzsche PC. Placebo interventions for all clinical conditions. Cochrane Database Syst Rev. 2010;2010(1):CD003974. Published 2010 Jan 20. doi:10.1002/14651858.CD003974.pub3
Rubinstein S M, de Zoete A, van Middelkoop M, Assendelft W J J, de Boer M R, van Tulder M W et al. Benefits and harms of spinal manipulative therapy for the treatment of chronic low back pain: systematic review and meta-analysis of randomised controlled trials BMJ 2019; 364 :l689 doi:10.1136/bmj.l689