Aging or De-Conditioned?
"This is just part of getting older."
"I'm just getting older, not able to do what I used to do."
"Just give it a few years and you'll be in the same spot."
"I sure can't move like I used to."
We've all heard these phrases or maybe even said them ourselves. It's true that as we age, our bodies change and we may not be able to do everything we once could. However, how much of that is truly due to the inevitable aging process, and how much of it is a result of deconditioning from a lack of regular physical activity?
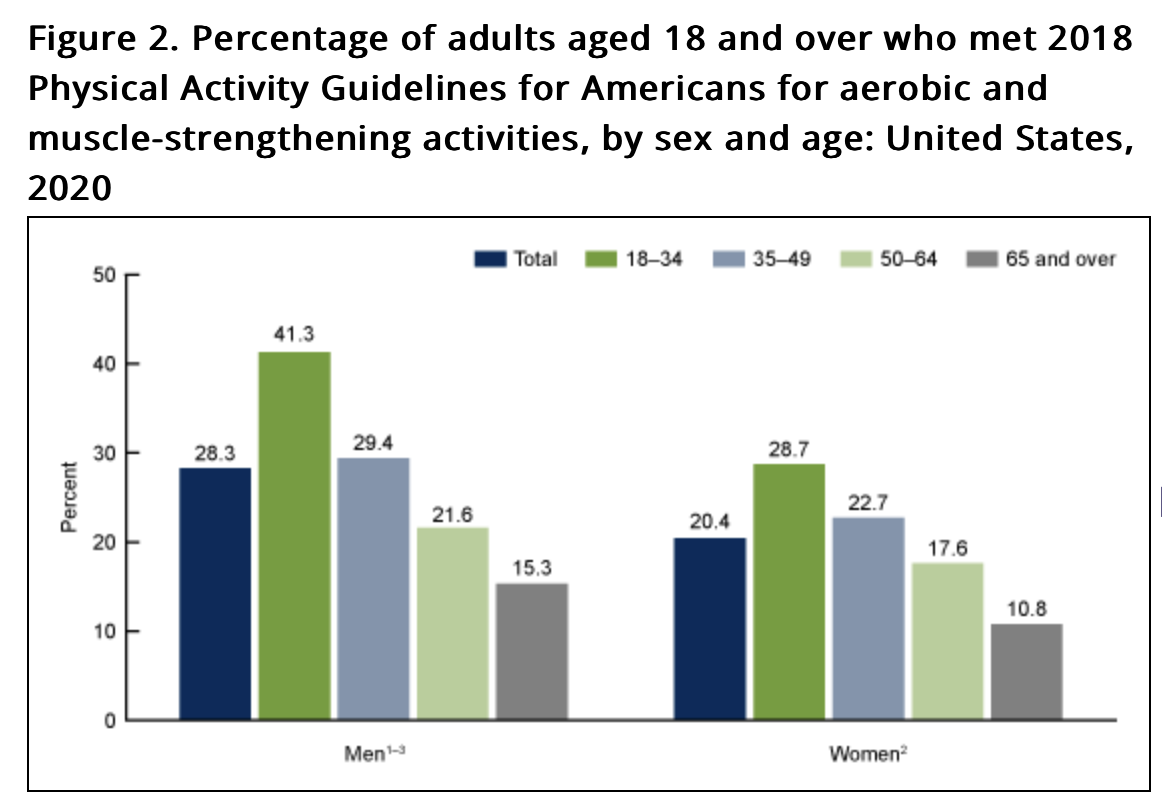
We've all seen the 30 year old that looks and moves like they're 50 and the 50 year old that looks and moves like they're 20. Much of that difference comes down to lifestyle habits, especially physical activity and exercise. For most of us, we are the most active in elementary and middle school. Then activity levels tend to decrease in high school, college, and especially by our mid-30s as work, family and life commitments take over our time and energy. On the right you can see the percentage of adults who met physical activity guidelines for aerobic and muscle-strengthening activities.
There are a multitude of reasons that we decrease our movement and physical activity as we age. Maybe movement wasn't part of your childhood, maybe you had horrible coaches and after middle school or high school you decided you were done moving. Or maybe life just got busy, like it does for so many of us, and movement became lower and lower on the list of priorities with work, kids, and other responsibilities taking over your time.
This gradual decrease in movement leads to deconditioning of our muscles, tendons, ligaments, heart, veins, arteries and lungs. When these tissues are not regularly challenged with physical activity, they slowly lose strength, elasticity, and capacity to function. Muscles get smaller and the symbiotic relationship between our endurance muscle fibers and our power muscle fibers decreases as the power fibers decrease. Tendons and ligaments become less resilient. The heart's ability to pump blood efficiently declines. Arteries stiffen and are more prone to plaque buildup. Lung capacity and oxygenation decrease.
What exactly is deconditioning?
Deconditioning looks different for all of the tissues mentioned above, but in essence, it is a tissue's slow loss of overall function due to lack of use. This occurs because most of our tissues need to be utilized regularly to maintain their health and optimal function.
Muscle Deconditioning
For our muscles, deconditioning involves the transition from a mix of type 1 (slow/endurance) and type 2 (fast/strength) muscle fibers to primarily type 1 fibers. There is also a decrease in the sensors of the muscles called mechanoreceptors. As this occurs, our accuracy of movement decreases and our ability to move quickly and lift heavy things decreases. Additionally, there is a decrease in mitochondria, the powerhouses of the cell, meaning if we have fewer mitochondria in our muscle cells, they tire more easily.
Heart Deconditioning
When the heart becomes deconditioned, the heart muscle (myocardium) begins to atrophy, leading to a decrease in the thickness of the heart walls. This atrophy is caused by a reduction in the size and number of individual heart muscle cells, known as cardiomyocytes. There is also a decrease in the number of mitochondria within the cardiomyocytes, resulting in reduced energy production and a decreased ability to generate force during contractions. The heart's electrical conduction system may also be affected, leading to abnormalities in heart rhythm. Overall, these changes lead to a reduction in the heart's ability to pump blood efficiently, resulting in lower cardiac output and reduced cardiovascular fitness. Another aspect of the heart losing its healthy condition is increased stiffness where the heart can’t properly relax to allow the heart to fill with blood before it contracts to pump blood. This leads to a decrease in the amount of blood that can be sent to the rest of the body and to compensate for reduced filling, the pressure in other parts of the heart increases, which can lead to symptoms of congestive heart failure, such as shortness of breath (dyspnea), especially during exertion. Overtime this leads to an increase risk of heart attack and stroke.
Lungs Deconditioning
Deconditioning of the lungs leads to several physiological changes that affect respiratory function. The alveoli, the tiny air sacs responsible for gas exchange, may become less elastic and have a reduced surface area, leading to decreased oxygen uptake and carbon dioxide removal. The respiratory muscles, including the diaphragm and intercostal muscles, can atrophy and weaken, making it more difficult to take deep breaths and leading to a decrease in lung volumes and capacities. Additionally, the pulmonary capillaries surrounding the alveoli may become less dense, further reducing the efficiency of gas exchange. These changes can result in a reduced ability to oxygenate the blood and remove carbon dioxide, leading to shortness of breath and reduced exercise tolerance.
Tendon and Ligaments Deconditioning
Tendons and ligaments also undergo changes with deconditioning. These connective tissues are primarily composed of collagen fibers, which provide strength and elasticity. When tendons and ligaments are not subjected to regular mechanical stress through physical activity or movement, the collagen fibers become disorganized and less dense. This leads to a reduction in the tissues' tensile strength and ability to store and release elastic energy. Additionally, the fibroblasts responsible for maintaining and repairing these tissues become less active, leading to a decreased ability to adapt to mechanical stress and repair micro-damage. As a result, tendons and ligaments become more susceptible to injury and have a reduced capacity to handle the demands of physical activity.
Veins and Arteries Deconditioning
Deconditioning of veins and arteries can have significant implications for cardiovascular health. The endothelium, the inner lining of blood vessels, plays a crucial role in regulating vascular tone and blood flow. When the endothelium becomes deconditioned, it may have a reduced ability to produce nitric oxide, a molecule that helps blood vessels dilate and maintain healthy blood flow. This can lead to increased vascular resistance and a reduced ability to respond to changes in blood flow demand. Additionally, the smooth muscle cells in the walls of blood vessels may atrophy and become less responsive to signals that regulate their contraction and relaxation. This can further contribute to reduced vasodilation and increased vascular stiffness. Over time, these changes can lead to the development of atherosclerosis, a condition characterized by the buildup of fatty plaques in the arterial walls, which can increase the risk of heart attack and stroke.
What Can We Do About Deconditioning?
As we decrease our activity we become more deconditioned, the body's tissues are simply not prepared to handle higher intensity activities. This can then lead to injuries, pain, and an overall discouragement when you do try to push yourself. It becomes a vicious cycle of less movement leading to more deconditioning.
However, a landmark study has shown that it's possible to break this cycle and reverse the effects of deconditioning, even in middle age.
The study set out to determine if starting an optimized exercise training program in middle age could reverse the deleterious cardiac effects of sedentary aging. The researchers hypothesized that 2 years of exercise training, including high-intensity intervals, started in middle age, may be an effective strategy to reduce age-related increases in cardiac stiffness - a key factor in the development of heart failure due the increased stiffness we discussed earlier that starts to occur in the heart due to inactivity.
Reversing the Cardiac Effects of Sedentary Aging in Middle Age—A Randomized Controlled Trial
The study was designed as a prospective, parallel-group, randomized controlled trial. Sixty-one sedentary, middle-aged participants were randomly assigned to either 2 years of exercise training or a control group doing balance and flexibility training. The exercise training was individually prescribed and progressed over time, including high-intensity intervals, moderate-intensity continuous exercise, and strength training. Participants gradually increased their training to 5-6 hours per week, a significant time commitment but one that is in line with current physical activity guidelines for optimal health. Extensive physiological testing, including invasive pressure-volume measurements, was conducted at baseline and after the 2-year intervention to assess changes in cardiac function.
The results of the 2-year exercise training intervention were remarkable. Exercise capacity, as measured by VO2max, increased by a whopping 18% in the exercise group, while there was no change in the control group. This is a clinically significant improvement that would be expected to substantially reduce the risk of cardiovascular events and mortality. Even more impressively, left ventricular stiffness significantly decreased in the exercise group, whereas it did not change in controls. The exercise group also had increased left ventricular end-diastolic volume, allowing for greater stroke volume at any given filling pressure - an improvement in Frank-Starling reserve, which is a key determinant of cardiovascular performance during exercise. Importantly, these changes occurred without alterations in cardiac systolic function, suggesting that the benefits were primarily driven by improvements in diastolic function.
This study provides the first direct evidence that sedentary, middle-aged adults can reverse the effects of sedentary aging on the heart with a prolonged, optimized exercise training program. The results support recommending at least 150 minutes per week of varying intensity exercise to reduce the risk of heart failure development. For middle-aged adults, it's not too late to start exercising to achieve a healthier better conditioned heart. Endurance exercise, including some high intensity training, is a powerful stimulus to reduce cardiac stiffening and improve cardiovascular function. The earlier you can incorporate this into your routine, the better, but middle age is not too late to see meaningful benefits.
So before assuming that your aches, pains and limitations are "just part of getting older," consider whether a lack of regular challenging exercise is the real culprit. By prioritizing movement and embracing physical challenges, you can take control of how your body ages and enjoy the vitality and freedom to keep doing what you love for years to come. Getting older is inevitable, but deconditioning doesn't have to be.
Here are the specifics of the training that was done in the research.
Please Click here for a 6 Month - Weekly Calendar showing you what to do each day over a 6 month period. For individuals in the research after the 6 months of training they maintained the same level of training of month 6 for the remaining 4 months. “After completion of the 10-month progression, exercise capacity was retested and then participants began the maintenance training phase. Training zones were adjusted to reflect the results of the most recent exercise test. During this period, participants performed only 1 interval session per week plus continuous training. Participants were encouraged to use a variety of exercise equipment (eg, stationary cycle ergometer, treadmill, elliptical trainer) or perform exercise sessions outdoors (eg, running on trails, cycling, swimming) to ensure participant enjoyment and to avoid overuse injuries. To supplement the endurance train- ing, 2 weekly strength training sessions were prescribed. These sessions were designed to focus on whole body functional and core strength to complement the endurance training.”
The following 6 month cardiovascular workout plan is based off of the 2018 study Reversing the Cardiac Effects of Sedentary Aging in Middle Age—A Randomized Controlled Trial Implications For Heart Failure Prevention.
Heart Rate Max Can be Calculated Utilizing the following equation: HRmax=208−(0.7×age)
4 Training Zones will be utilized in this 6 month plan: (1) MSS ; (2) Base pace (1–20 beats below MSS); (3) Interval (>95% HR peak); and recovery (<base pace)
MSS or Maximal Steady State: Step-by-Step Calculation for MSS Zone:
Determine HRmax:
Calculate 75% of HRmax: This percentage often aligns with the lower end of the MSS zone, suitable for longer, sustained efforts.
HR Max × 0.75 = 75% of HRmax
Calculate 90% of HRmax: This percentage is closer to the upper limit of the MSS zone, where effort is more intense but still sustainable.
HR Max × 0.90 = 90% HR Max
Base pace (1–20 beats below MSS) There will be some overlap in Base Pace and MSS, if you notice in the later weeks there are less base pace days, this is for you to determine how much you can push yourself based on your recovery after the interval days.
Interval (>95% HR peak). On these days, intervals will consist of 4×4 interval sessions (4 minutes of exercise at 95% peak HR followed by 3 minutes of active recovery at 60%–75% peak HR, repeated 4 times)
Month 1:
3 base pace sessions per week, 30 minutes each
Month 2:
3 base pace sessions per week, 30 minutes each
2 MSS (Maximum Steady State) sessions per month
Month 3:
3 base pace sessions per week, 30 minutes each
3 MSS sessions per month
1 aerobic interval session (4×4 interval) per week, followed by a recovery day of 20-30 minutes walking or light aerobic activity
Month 4:
3 base pace sessions per week, 30 minutes each
3 MSS sessions per month
1 aerobic interval session (4×4 interval) per week, followed by a recovery day of 20-30 minutes walking or light aerobic activity
Training load gradually increases towards 5-6 hours per week
Month 5:
2 aerobic interval sessions (4×4 interval) per week, each followed by a recovery day of 20-30 minutes walking or light aerobic activity
1 long session (at least an hour) per week
1 base pace session, 30 minutes
Training load reaches 5-6 hours per week
Month 6:
2 aerobic interval sessions (4×4 interval) per week, each followed by a recovery day of 20-30 minutes walking or light aerobic activity
1 long session (at least an hour) per week
1 base pace session, 30 minutes
Training load maintained at 5-6 hours per week
As always I hope you enjoyed this blog and if you have any questions at all please feel free to reach out to me at drcoffman@optimizecolumbus.com.