Decoding Headaches: The Pivotal Role of Balance
Balance & Headaches
Balance is a fundamental concept that shapes our daily lives. From standing on one foot to trying not to fall while riding a bicycle, it's a concept we understand intuitively. What we might not fully comprehend is the complex systems within our bodies that maintain this equilibrium and how disruptions to these systems can lead to certain health conditions like headaches, neck pain, and dizziness.
Headaches, while seemingly simple, are far from being just one single condition. They are, in fact, categorized into various types, each with its unique characteristics and triggers. The most prevalent among these are migraines and tension-type headaches (TTH). Migraines often characterized by throbbing pain, are usually but not always, accompanied by symptoms such as sensitivity to light and sound, and occasionally nausea. Tension-Type Headaches on the other hand, are more chronic and can be felt as a constant pressure around the forehead or back of the head and neck.
However, these categories aren't mutually exclusive, and there's considerable overlap in their symptomatology and where they come from. Some patients may experience both types at different times, further complicating their diagnosis and management. The common thread among these conditions, however, is their potential to significantly diminish a person's quality of life and their contribution to global disability. Intriguingly, these types of headaches also share a peculiar connection to our perception of balance and verticality - a link we're beginning to unravel and what we’ll be primarily discussing in todays blog.
The Triad of Balance
Firstly, let's consider the three systems that regulate our balance - the visual, vestibular, and proprioceptive systems.
Our visual system provides us with a perception of our environment, defining our position relative to the objects around us. The vestibular system, located in our inner ear, is our biological compass that responds to gravitational forces and keeps us upright, it does this by fluid that moves around in three different canals in our inner ear. Lastly, the proprioceptive system involves the muscles and joints, which send signals to our brain about our body's position, helping us understand where our limbs are in space without having to look, close your eyes and touch your nose with your finger, that’s your proprioceptive system at work.
These systems function together to allow us to move seamlessly through our world. Yet, disruptions or imbalances within one of these systems can lead to a range of conditions. Research has linked imbalances in these systems to symptoms such as dizziness, neck pain, and headaches.
Dizziness can arise when there is a mismatch of information between these three systems.
Neck pain can occur when the proprioceptive system is disrupted, causing a poor sense of body positioning and leading to strain and overuse of the neck muscles.
Similarly, headaches, particularly migraines and tension-type headaches, have been linked to these disruptions. The pain we experience in a headache can be a result of overcompensation, adaptation, or lack of proper function in one or more of these systems. Although these imbalances can manifest in various ways, the focus of our discussion today will be on how they relate specifically to headaches. Understanding this connection provides us with the capability to fine tune the treatment of these widespread and debilitating conditions
Robust but not Indestructible.
These systems, while robust, are not invincible. Trauma, especially to the neck, can have a profound impact on these systems and our balance. Imagine a whiplash injury, often occurring in car accidents or high-impact sports incidents. The violent backward and forward motion can injure the muscles and ligaments in the neck. This can lead to inflammation, reduced range of motion, and pain - factors that can disrupt the proprioceptive system, altering our sense of body position and subsequently affecting our balance.
A key aspect that links neck trauma to balance disorders is the alteration of the cervical-ocular reflex (COR). The COR is an essential reflex that stabilizes our gaze as we move our heads. This reflex is intricately tied to the neck's proprioceptive input, with receptors in the neck muscles, specifically the upper cervical spine, providing the necessary information for this reflex to function. However, post-trauma, especially following a whiplash injury, this reflex can be disturbed. There's often an increase in the COR gain - the ratio of eye movement to neck movement - leading to symptoms such as dizziness and unsteadiness, and further exacerbating the potential for headaches. When trauma to the neck occurs the delicate interplay between our neck muscles and our eyes is disrupted, making even the most mundane tasks a challenging feat for the head and the neck.
The Integral Role of the Upper Cervical Spine
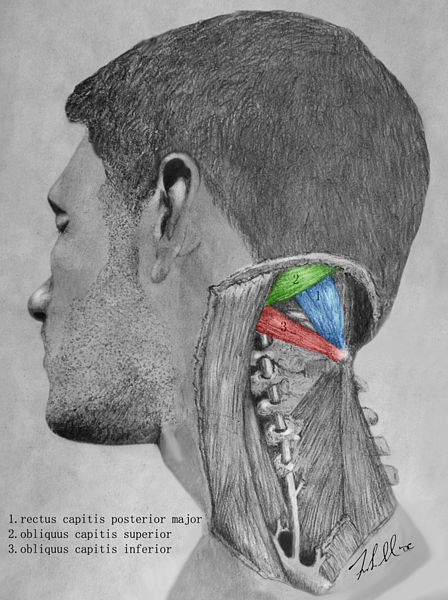
The upper cervical spine, located at the base of our skulls, has a fundamental role in our overall balance. This region is where small muscles known as the sub-occipital muscles live. Their unique characteristic lies in their wealth of muscle spindles, sensory receptors that provide the brain with detailed information about the position and movement of the head and neck.
It is due to this density of muscle spindles that the upper cervical spine has earned a reputation as a 'sensory organ' more than just a set of muscles. It forms a crucial network where the proprioceptive, visual, and vestibular systems intersect, each depending on the information relayed by this region to maintain a sense of balance and normal movement.
The role of the visual system is to provide us with a perception of our environment and our position within it. The vestibular system, located in our inner ear, responds to gravitational forces to keep us upright. The proprioceptive system, largely influenced by the health and function of the upper cervical spine, sends signals to our brain about our body's position. All these systems are in constant communication, working in harmony to maintain balance.
When the upper cervical spine is healthy, our perception of verticality, or how we perceive ourselves relative to gravity, remains precise. However, when this area is compromised due to injury or misalignment, it can lead to a cascade of problems. The incorrect sensory information produced by a misaligned upper cervical spine can cause the brain to miscalculate our body's positioning, affecting our balance and inducing symptoms such as dizziness and headaches.
Proper function and health of the upper cervical spine, therefore is crucial not just for our neck mobility, but also for the overall balance and spatial orientation of our bodies.
The Cycle of Imbalance: Understanding the Interplay of Headaches and Visual Vertical
The intricate interplay of various systems responsible for our orientation and balance means that a dysfunction in one can often lead to issues in others. This interconnectedness is particularly noticeable in patients suffering from primary headache disorders (PHD). In fact, a consistent observation in the research has been that individuals with headaches frequently exhibit a distorted perception of visual vertical. Intriguingly, this deviation is even more pronounced among those diagnosed with tension-type headaches (TTH).
The intricate interplay between our upper cervical spine, visual, and vestibular systems lays the foundation for understanding why disruptions in these systems can influence our perception of verticality and contribute to headaches. One significant aspect of this interplay is the role of our 'Subjective Visual Vertical' (SVV), which is our perception of what's vertical. Picture the Leaning Tower of Pisa. Even though it's visibly leaning, our brain makes a quick compensation, and we can still orient ourselves correctly in relation to it..
The upper cervical spine, with its rich network of proprioceptive receptors, plays a vital part in maintaining SVV. Any dysfunction in this area, such as due to trauma or muscle strain, can interfere with SVV and ultimately lead to altered function. The information from our cervical, vestibular, and visual structures converges and works harmoniously to determine this sense of verticality. A disruption to this delicate balance can lead to misperceptions of verticality, a phenomenon that is increasingly being linked to primary headache disorders (PHD)
This skewed perception of verticality likely originates from the underlying physiological processes associated with these disorders. Activities that generate neck pain or demand significant visual attention are common triggers for primary headaches. Given that the neck is densely populated with proprioceptive receptors, any disturbance in the upper cervical region's function can provoke both headaches and a misperception of verticality.
Oculomotor disturbances, or problems associated with eye movements, represent another significant component of this equation. These are prevalent among individuals with tension-type headaches and can lead to alterations in the ocular tilt reaction (OTR), a crucial mechanism that helps maintain an accurate perception of vertical. When OTR is affected, the person's perception of verticality may be distorted, leading to the onset of headaches.
Interestingly, there seems to be a cyclical relationship between headaches and vertical misperceptions. That is, not only can an altered perception of verticality trigger a headache, but the presence of a headache can further exaggerate these misperceptions. This feedback loop creates a vicious cycle, making the management of such conditions more complex.
Recent research has underscored the potential long-term impact of these issues. Continuous oculomotor disturbances and prolonged verticality misperceptions may lead to a chronic state of imbalance. Over time, this imbalance can make an individual more prone to further headaches, perpetuating the cycle of pain and imbalance. The interconnectedness of these systems underscores the importance of a holistic approach in treating such conditions.
Unraveling the Complications of Balance and Headaches
Our vestibular system plays a pivotal role in maintaining our balance and spatial orientation, but its role extends beyond just these functions. In individuals experiencing migraines, the vestibular system becomes intertwined with the pain pathways. Interestingly, these vestibular disorders don't simply exist as isolated health issues occurring alongside headaches. Instead, they could be integral manifestations of the headache itself, further complicating the relationships among these systems.
On a broader level, understanding the complex dance between these three systems—visual, vestibular, and proprioceptive—provides valuable insights into the cause of headaches and provides a path for treatment. When these systems are in perfect harmony, our perception of verticality is accurate, and we maintain our balance effortlessly. However, a disruption in any of these systems, as seen in patients with primary headache disorders, could lead to a misperception of SVV, resulting in debilitating conditions such as migraines and tension-type headaches.
These observations highlight the dynamic complexity of these systems and their potential roles in the onset and exacerbation of headache disorders. While a balance exists in healthy individuals, a 'tipping point' appears to be reached in those with primary headache disorders, where the balance is disrupted, leading to a cycle of chronic headaches and impaired balance.
Notably, the detailed exploration of these links uncovers potential treatment strategies. For instance, addressing these dysfunctions directly, what we do with our Data-Driven approach, can prove to be beneficial in mitigating the severity and frequency of these headaches and it many cases lead to complete resolution.
In conclusion, our perception of verticality goes beyond simply being an intuitive sense of balance. It's a complex mechanism involving a delicate interplay between our visual, vestibular, and proprioceptive systems. Any disruption, such as the misperception of vertical in headache disorders, can lead to widespread and disabling conditions like migraines and tension-type headaches.
At Optimize Chiropractic we understand how frustrating disorders like headaches, migraines, and dizziness can be. That’s why we exist, to help individuals with these issues find relief and get back to living the life they deserve.
As always I hope you enjoyed this blog and if you or someone you know suffers with headaches and think they’d benefit from reading this blog or benefit from care with us please share and as always you can reach me at drcoffman@optimizecolumbus.com.
References