Why Does Pain Linger After You Heal?
Last week I had the opportunity to present on the topic of Pain Neuroscience to the Rotary Club I belong to.
Pain Neuroscience answers the question: "Why does pain linger even after you heal?"
When we learn about pain we have: less fear around movement, enjoyment of more activities, less anxiety around pain, and we get better faster when combined with chiropractic, rehab, or physical therapy.
You can click this link to watch the full video or join us on May 20th from 5-6pm at the Friends theater of the Upper Arlington Library Tremont Branch where I'll be sharing about this topic again.
If you don't have time to watch the video or join us on May 20th I outlined 10 of the key concepts below - while pain neuroscience is a little more complicated than this - these 10 key concepts are the foundation of the neuroscience of pain.
10 Key Concepts About Pain: What Modern Science Tells Us
1. Pain as Protection
Pain isn't the enemy – it's our body's built-in alarm system. When my daughter eventually discovers our cast iron skillet's handle sticking out from the stove, that pain signal will teach her to avoid hot surfaces. We actually want that warning system! The problem comes when our alarm gets too sensitive, like a house alarm going off when a squirrel runs by. Pain exists(when working properly) to protect us, not punish us.
2. Context Matters
Our brains interpret signals differently based on context, and this explains a lot about how pain works. I grew up in Oklahoma where tornado sirens mean only one thing: immediate danger - get to the shelter because there's a funnel cloud nearby. When I moved to Ohio and first heard that same siren at night, my response was immediate panic - I woke my wife up saying we needed to get to the basement NOW.
She looked at me like I was crazy. "What are you talking about?" I quickly learned in Ohio, those sirens go off even when it isn't time to get into the shelter.
Another way to think about it is when that same siren goes off at noon on Wednesday in Upper Arlington, nobody panics. Same exact sound, but in that context, everyone knows it's just a routine test. It's not a signal of danger, so nobody feels fear.
Pain works in a similar manner. It's not just about the physical sensation - it's about how our brain interprets that sensation based on context. Sometimes our body feels pain when nothing is actually wrong, and sometimes significant damage occurs with no pain at all. Just like that siren can mean "immediate danger" or "just a test" depending on when and where it happens, the same physical sensation in your body can register as debilitating pain or barely noticeable discomfort depending on your stress levels, past experiences, previous injuries and how those injuries progressed, beliefs about your body, and dozens of other contextual factors.
3. The Disconnect Between Imaging and Pain
The truth about imaging findings is shocking – 37% of pain-free 20-year-olds have disc degeneration, and by 60, that number jumps to 88%! Even more surprising are studies showing "bad" shoulders often have the same MRI findings as pain-free shoulders in the same person. In some cases, there were MORE labrum alterations in the pain-free shoulder! What shows up on an MRI isn't necessarily what's causing your pain.
4. The Danger-Safety Balance
Pain happens when our brain's “scale” tips toward "danger" rather than "safety." So many factors influence this balance – tissue damage, yes, but also stress hormones, fearful thoughts, past injuries, and even how healthcare providers explain our condition. When someone in a white coat points to an x-ray and says "this is terrible," that alone can tip your scale toward danger and increase pain.
5. The Orchestra of Pain
There's no single "pain center" in our brain. Instead, pain involves multiple brain regions working together like an orchestra. When we experience chronic pain, our brain creates neural grooves – like cattle paths worn into a field after repeated use – making pain our "new normal." These well-worn neural pathways can keep sending pain signals even when there's no danger. That's why simply addressing tissue isn't enough.
6. Movement as Medicine
The brain is neuroplastic – it can change and create new neural pathways. When we gradually introduce movement in a safe way, we're essentially teaching our brain that movement doesn't equal danger. Research on walking programs for back pain, where participants increased walking by just 10% weekly, proves this point. Movement helps rewire the brain's understanding of what's safe versus dangerous. Just like the cattle path metaphor above, these neural paths can be changed and chronic pain can improve.
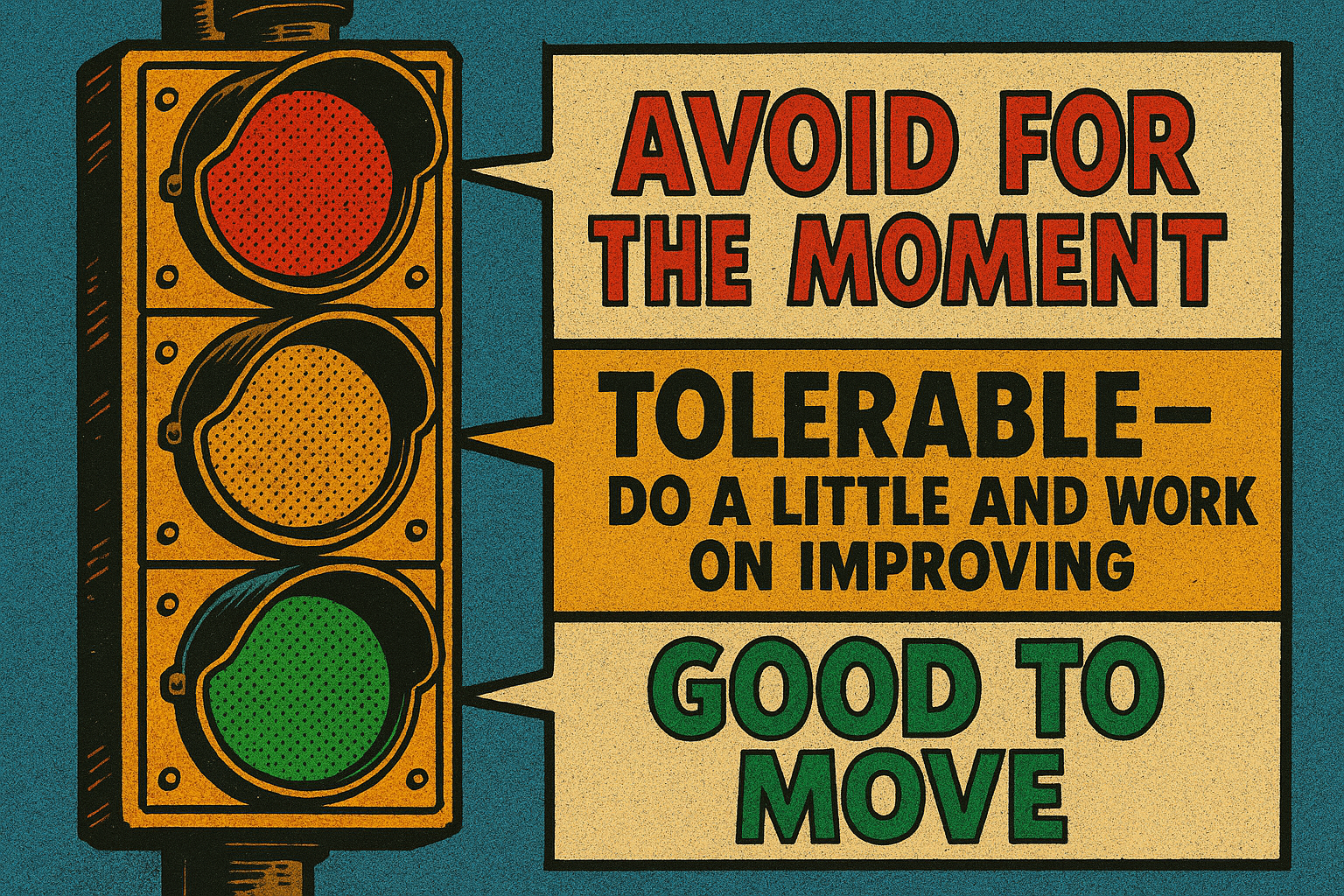
7. The Stoplight Approach to Movement
Think of your movements like a traffic light:
Green movements feel good – do these freely
Yellow movements are tolerable but can get uncomfortable if overdone – do these in moderation
Red movements cause pain – avoid these for now
The magic happens when you consistently do your greens, carefully incorporate yellows, and avoid reds. Over time, your yellows become greens, and your reds become yellows. This creates a gradual expansion of pain-free movement.
8. The Deconditioning Trap
When something hurts, we naturally avoid using it. But this creates a dangerous cycle – the shoulder that hurts gets used less, causing those muscles and tendons to weaken. Meanwhile, we compensate with other body parts. Then when we try to use that shoulder again, it's not ready for the load, gets sore, and we think, "I've re-injured it!" This leads to more avoidance, more weakness, and an ongoing cycle of pain.
9. The Acute-Chronic Workload Ratio
This is something sports scientists use that we should all know about. Your injury risk skyrockets when you suddenly do more than 50% more activity than your average over the past four weeks. This is why we get hurt in spring doing yard work after being inactive all winter. Our tissues need gradual loading to adapt and strengthen, not sudden spikes in activity.
10. Go Slow and Be Consistent
If an hour of gardening aggravates your back, start with 30 minutes. Set a timer. Take breaks. Come back to it later. This isn't giving up – it's being strategic. The goal is to gradually build the "safety in me" rather than the "danger in me." Consistency with manageable doses of activity will get you much further than pushing through pain, then spending a week recovering.
References
Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811-816. doi:10.3174/ajnr.A4173
Di Maio G, Villano I, Ilardi CR, et al. Mechanisms of Transmission and Processing of Pain: A Narrative Review. Int J Environ Res Public Health. 2023;20(4):3064. Published 2023 Feb 9. doi:10.3390/ijerph20043064
Galán-Martín MA, Montero-Cuadrado F, Lluch-Girbes E, Coca-López MC, Mayo-Iscar A, Cuesta-Vargas A. Pain neuroscience education and physical exercise for patients with chronic spinal pain in primary healthcare: a randomised trial protocol. BMC Musculoskelet Disord. 2019;20(1):505. Published 2019 Nov 3. doi:10.1186/s12891-019-2889-1
Goudman L, Huysmans E, Ickmans K, et al. A Modern Pain Neuroscience Approach in Patients Undergoing Surgery for Lumbar Radiculopathy: A Clinical Perspective. Phys Ther. 2019;99(7):933-945. doi:10.1093/ptj/pzz053
Greenwald JD, Shafritz KM. An Integrative Neuroscience Framework for the Treatment of Chronic Pain: From Cellular Alterations to Behavior. Front Integr Neurosci. 2018;12:18. Published 2018 May 23. doi:10.3389/fnint.2018.00018
Hillier S, Immink M, Thewlis D. Assessing Proprioception: A Systematic Review of Possibilities. Neurorehabil Neural Repair. 2015;29(10):933-949. doi:10.1177/1545968315573055
Lee CH, Chen CC. Role of proprioceptors in chronic musculoskeletal pain. Exp Physiol. 2024;109(1):45-54. doi:10.1113/EP090989
Louw A, Zimney K, O'Hotto C, Hilton S. The clinical application of teaching people about pain. Physiother Theory Pract. 2016;32(5):385-395. doi:10.1080/09593985.2016.1194652
Nijs J, Clark J, Malfliet A, et al. In the spine or in the brain? Recent advances in pain neuroscience applied in the intervention for low back pain. Clin Exp Rheumatol. 2017;35 Suppl 107(5):108-115.
Nijs J, Meeus M, Cagnie B, et al. A modern neuroscience approach to chronic spinal pain: combining pain neuroscience education with cognition-targeted motor control training. Phys Ther. 2014;94(5):730-738. doi:10.2522/ptj.20130258
Peng B, Yang L, Li Y, Liu T, Liu Y. Cervical Proprioception Impairment in Neck Pain-Pathophysiology, Clinical Evaluation, and Management: A Narrative Review. Pain Ther. 2021;10(1):143-164. doi:10.1007/s40122-020-00230-z
Plaut S. Scoping review and interpretation of myofascial pain/fibromyalgia syndrome: An attempt to assemble a medical puzzle. PLoS One. 2022;17(2):e0263087. Published 2022 Feb 16. doi:10.1371/journal.pone.0263087
Salamanna F, Caravelli S, Marchese L, et al. Proprioception and Mechanoreceptors in Osteoarthritis: A Systematic Literature Review. J Clin Med. 2023;12(20):6623. Published 2023 Oct 19. doi:10.3390/jcm12206623
Salazar-Méndez J, Cuyul-Vásquez I, Ponce-Fuentes F, et al. Pain neuroscience education for patients with chronic pain: A scoping review from teaching-learning strategies, educational level, and cultural perspective. Patient Educ Couns. 2024;123:108201. doi:10.1016/j.pec.2024.108201
Taylor JL, Amann M, Duchateau J, Meeusen R, Rice CL. Neural Contributions to Muscle Fatigue: From the Brain to the Muscle and Back Again. Med Sci Sports Exerc. 2016;48(11):2294-2306. doi:10.1249/MSS.0000000000000923
Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. BMJ. 2015;350:h2747. Published 2015 Jun 16. doi:10.1136/bmj.h2747
Zeng CY, Zhang ZR, Tang ZM, Hua FZ. Benefits and Mechanisms of Exercise Training for Knee Osteoarthritis. Front Physiol. 2021;12:794062. Published 2021 Dec 16. doi:10.3389/fphys.2021.794062
Zheng Q, Dong X, Green DP, Dong X. Peripheral mechanisms of chronic pain. Med Rev (2021). 2022;2(3):251-270. doi:10.1515/mr-2022-0013